Treatments
My Rao practices are mainly lower limb orthopaedic and trauma surgery. His expertise is in primary hip and Knee replacement as well as in Revision or re-do Hip and Knee arthroplasty surgeries.
Hip Replacement Surgery
Total hip replacements are among the most successful Orthopaedic surgeries having a positive impact on health-related quality of life. Hip and knee replacements primarily relieve pain but are also known to maximise function in everyday life and to reach a higher level of well-being.
Mr. Rao practices both minimal invasive and standard hip replacement surgery. He uses his implants according to the personal needs of patients. He uses cemented, hybrid, uncemented to dual mobility hip replacements and from ceramic on ceramic articulations in younger patients to ceramic on polyethylene to metal on polyethylene joint articulations as per patient requirements.
Mr. Rao is experienced in doing complex primary hip replacement including for dysplastic hips. He also does simultaneous bilateral hip replacements according to patient pathology.
Patient Resources:

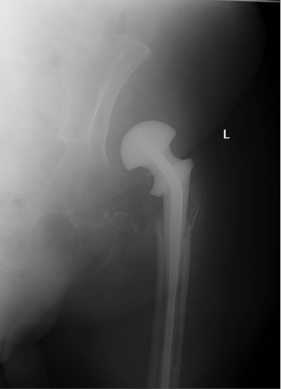
Right Hip Osteoarthritis

Hybrid Hip Replacement

Left Hip Osteoarthritis

Uncemented Hip Replacement

Bilateral Ankylosing Spondylitis of Hips

Simultaneous Bilateral hip replacements

Failed fracture neck of femur fixation

Complex total hip replacement
Knee Replacement Surgery
Knee is most commonly replaced joint and is required when knee pain becomes disabling, constant and interferes with your common activities of daily life. Most common cause for knee replacement is osteoarthritis and around 80-90,000 procedures are carried out in England, Wales, Northern Ireland and the Isle of Man annually.
This is a major operation during which the damaged joint surfaces are removed and replaced by a metal implant and a special plastic insert in between them. The aim of the procedure is to relieve pain and restore movement and function.
Mr Rao practices enhanced recovery and rehabilitation for this procedure. Following consultation, diagnosis and investigations, you will be admitted on the day of the surgery and will be walking either the same day or following day of the surgery. You will be in the hospital for about 3 nights. Recovery generally takes place in about 6 weeks but medical literature suggests that knee replacement patients can improve up to a year following surgery.
Patient Resources:
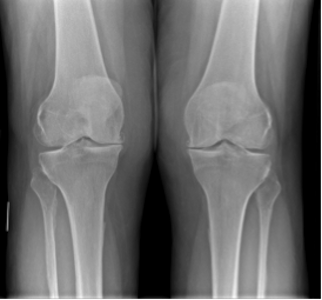
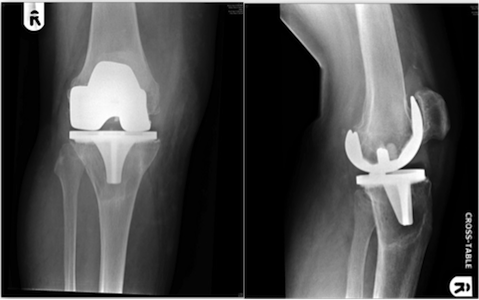
Bilateral Knee osteoarthritis
Post op Knee replacements
Unicompartmental / Partial Knee Replacements
The knee is divided into three compartments - Medial (inner half), Lateral (Outer half) and Patello-Femoral (Knee cap with Femur). The inner half of the joint between the thigh bone (femur) and shin bone (tibia) is called the medial compartment and outer half the thigh bone (femur) and shin bone (tibia) is called the lateral compartment. The Knee cap articulating with front of femur is called Patello-Femoral joint. Arthritis affecting only parts of knee or one compartment can be replaced in isolation without disturbing the other parts of knee joint.
Unicompartmental or partial knee replacement is a surgical procedure in which only one of the diseased knee compartments is replaced. It can be either Medial Unicompartmental knee replacement, Lateral Unicompartmental knee replacement or Patello-Femoral joint replacement.
The advantage of partial knee replacement over total knee replacement is that the knee ligaments are all spared by the surgery and the parts of knee not affected by arthritis are not touched. This allows normal knee movement and a normal feeling in the knee. In addition the operation is carried out with a small incision and less trauma. The prosthesis does not interfere with existing ligaments, tendons, or nerves. You retain normal balance and the natural stability of the healthy half of your knee joint and your own tendons and ligaments. Your kneecap is left in place, enabling you to regain much of the strength in your quadriceps.
In general, Unicompartmental knee replacements involve smaller incisions, less bleeding, quicker recovery, and less bone loss than a total knee replacement.
Mr. Rao practices minimal invasive surgery through smaller incisions for Unicompartmental knee arthroplasty, which will reduce pain and have a shorter recovery period than a total knee replacement.
Patient Resources:
Patello-Femoral Joint replacement

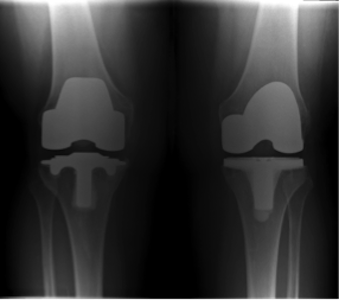
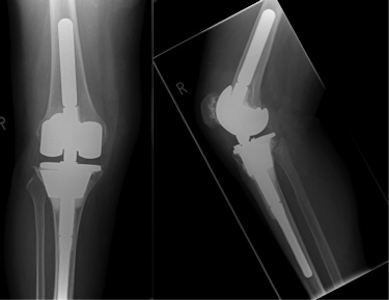
Preop X-Ray of Medial compartment OA

Post op X-Ray of medial Unicompartmental knee replacement
Complex Revision Hip Replacements (Redo Hip Replacement)
Modern technologies have made hip replacements to last longer and longer but still they can wear out in 15-20 years and lead to condition called aseptic loosening. The most common presenting symptom for this condition will be pain and instability. This is when one needs Revision Hip Surgery.
Infection in joint replacement though rare, is the other reason for one needing Revision Hip Surgery. One can do as one stage if bug infecting joint replacement is known or as a two staged procedure. This is a complex procedure where infected joint replacements firstly is removed at first instance and then at later stage the prosthesis have to be reinserted around 6-8 week mark, leaving patient in between two stages with a temporary hip spacer.
Other reasons hip replacement needing revisions can be when patients have recurrent dislocations of hips, fractures around hip replacements, ongoing pain and discomfort for mechanical problems like leg length discrepancy or offset problems and bone and muscle damage from their previous metal on metal hip replacements.
These procedures are more challenging for surgeons and patients alike, since typically there is more bones loss and tissues are inflamed or weak when they need to be replaced to the new components. Mr Rao is well experienced in these procedures and has been doing them for nearly a decade now.
Patient Resources:
http://www.arthritisresearchuk.org/arthritis-information/arthritis-today-magazine/159-winter-2013/the-challenge-of-revision-hip-replacement-surgery.aspx

Loosening of hip replacement

Revision Hip replacement

Failed multiple right revision hip replacements with bone loss and recurrent dislocations

Proximal Femoral replacement with complex acetabular reconstruction
Complex Revision Knee Replacements (Redo Knee Replacement)
A revision knee replacement surgery is a procedure that is performed to replace a knee implant that is no longer functioning properly. Most knee replacements last around 15 years and some longer. However, there are also times when a knee replacement needs to be redone after many years or even rarely earlier than that.
Some of the more common reasons needing revision knee replacement include Aseptic loosening of the implant, infection of the joint, instability of the knee, malalignment of the prosthesis and fractures around knee replacement.
Understanding why a knee replacement has worn out is critical to performing a successful revision knee replacement. When performing a revision knee, often some damaged bone has to be removed, and some may be lost as a result of the problem with the implant. Maintaining adequate bone to support the new implant can be challenging. Finally, obtaining a knee that is flexible enough to allow for motion, yet stable enough to keep you steady, is also more difficult in revision situations.
Mr Rao is well experienced in revision knee replacement surgery and has done immense work in dealing these bony defects using Trabecular Metal cones and modern implants. Mr Rao analyses each individual patient and offers the most appropriate solution for each patient.
Patient Resources:
http://www.arthritisresearchuk.org/arthritis-information/surgery/knee-replacement/different-types/complex-knee-replacement.aspx
http://orthoinfo.aaos.org/topic.cfm?topic=A00712
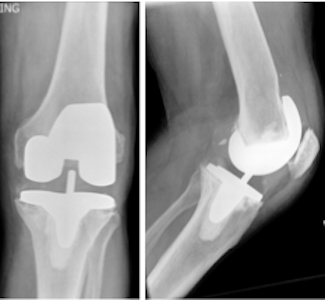
Pre op aseptic Loosening of Knee replacement
Post op X-ray of revision Knee replacement
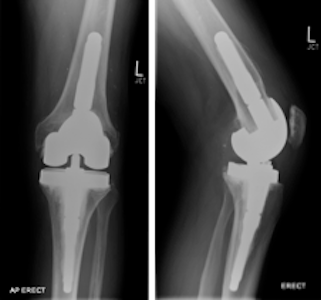
Aseptic Loosening of Knee replacement with large tibial bone defect
Revision Knee replacement with complex tibial reconstruction
Patello-femoral joint problems (Knee cap problems)
Patella (Knee cap) Realignment Procedures
There are many different actual reasons and factors that can cause or contribute to patellar (knee cap) malalignment. This can lead to pain in the knee, recurrent subluxation or dislocation of knee cap. It is essential that these be identified and quantified prior to any kind of treatment potentially being suggested. Mr. Rao offers careful and detailed clinical assessment and organises specialist imaging (X-rays, MRI, CT and/or ultrasound) to diagnose this problem. Following thorough assessment treatment can be offered either through conservative or surgical approach. There are many different surgical options available and Mr. Rao offers the most appropriate procedure. These can be either arthroscopic (key hole) or open surgical procedures.
Arthroscopy of knee - (keyhole surgery)
Arthroscopy is a common day surgery procedure carried out under general anaesthesia to treat various joint problems and knee is probably the commonest joint for this procedure. An arthroscopy involves the use of a telescope with camera to examine the knee joint through a small keyhole. Images are sent from the arthroscope to a video screen to be able to see inside the joint. Using other keyhole surgical instruments can be used alongside an arthroscope to allow treat certain joint conditions.
Meniscal injuries of knee
The meniscus is a piece of cartilage that provides a cushion between your thighbone (femur) and shinbone (tibia). There are two menisci in each knee joint. Medial (inner half of knee) and Lateral (outer half of knee).They can be damaged or torn during activities that put pressure on or rotate the knee joint. Taking a hard tackle on the football field or a sudden pivot on the basketball court can result in a meniscus tear. Sometimes you don’t have to be an athlete to get a meniscus tear, though. Simply getting up too quickly from a squatting position can also cause a meniscal tear. Depending on the pattern and extent of the tear, the arthroscopy may involve either a partial meniscectomy or meniscal repair. Mr Rao will examine and organise appropriate investigations (MRI, X-rays etc.) to come to a diagnosis. Following this he will carry out the necessary keyhole surgery. Depending on the procedure one can expect to be either fully weight bearing straight away or non-weight bearing for 4-6 weeks on the leg. Following arthroscopy, a rehabilitation and exercise program facilitates restoration of motion and strength.
Mr. Rao offers following services –
- Meniscal repairs
Most meniscal tears are treated by conservative trimming of the meniscus. However where there is a large peripheral tear there is a potential to undertake a repair.
- Partial meniscectomy/ Meniscal trimming or excision of tears
In this procedure, the damaged meniscus tissue is trimmed away.
- Removal of Loose bodies
Loose bodies are small loose fragments of cartilage or a bone that float around the knee joint The loose bodies can cause pain, swelling, and locking, and catching of the joint. Loose bodies are commonly found in individuals who participate in sports since they are more susceptible to fractures and other sports injuries. Other reasons for loose bodies in the knee can be due to osteoarthritis, rheumatoid arthritis, fractures, trauma, bone and cartilage inflammation. The loose bodies are removed by arthroscopic procedure. Surgery is performed depending on the location and the size of the loose bodies.
- Radiofrequency Chondroplasty
Articular cartilage damage in the knee is an extremely common problem. For young patients with partial thickness cartilage damage in a symptomatic joint, where the damage is not actually severe enough to contemplate major surgery, Mr. Rao uses highly useful and effective option of radiofrequency chondroplasty (otherwise known as coblation chondroplasty). This is carried out through keyhole and is a day case procedure. This very effectively smoothens off the surface of rough damaged cartilage and stabilizes the damaged tissue – much like using a blow torch to tidy up flaky paint peeling off a rusty gate. Smoothing off and properly stabilizing damaged articular cartilage surfaces does not make the cartilage grow back (articular cartilage has no blood supply and thus has extremely poor healing/regenerative capacity); however, it does reduce knee pain, thereby improving function, and it helps keeps patients’ knees going for longer, delaying the potential need for future bigger operations.
Patient Resources:
Microfracture technique and chondroplasty
Microfracture is a surgical option used in the treatment of areas of damaged cartilage. When a patient has a small area of damaged cartilage (not widespread arthritis), microfracture may be performed in an attempt to stimulate new cartilage growth. Microfracture is most often performed inside the knee joint.
How it works: Surgeons clean and smooth the cartilage tear’s edges and pierce holes in underlying bone, forming a blood clot rich in stem cells and growth factors. Over time, the clot remodels into fibrocartilage, which is less supple and durable than the original, hyaline cartilage.
http://www.orthopaedicsone.com/display/Main/Microfracture+Chondroplasty
Patient Resources:
ACL Reconstructions
The anterior cruciate ligament (ACL) is the main stabilising ligament at the front of the middle of the knee that stops the tibia translating forwards. The ACL also has a role in preventing rotational instability. ACL tears are relatively common in football, skiing or netball injuries, and tend to occur when the knee is twisted in a bent position, often in combination with impact/running. The immediate result of an ACL tear is severe pain and swelling in the joint. The longer-term results of having ACL deficiency in the knee are increased laxity (wobble), potential functional instability (giving way), increased risk of subsequent meniscal cartilage tears and an increased risk of arthritis in the knee.
ACL reconstruction is a highly successful operation done through key holes. A ‘graft’ is taken from patient either Hamstring tendon or bone patella bone tendon. Narrow tunnels are drilled through the tibia (shin bone) and the femur (thigh bone) into the middle of the knee. The ligament graft is passed up these tunnels, fixed at the top, tensioned and then fixed under tension at the bottom, to give a new tight ligament in the knee. With time, the new ligament grows a new blood supply in the knee, and the graft becomes a living structure within the patient’s knee.
Regular physio treatments will be needed, and particular from 3 months onwards patients are encouraged to spend lots of time in the gym doing specific exercises. Patients should not return to sport until 9 months post-op.
Patient Resources:
http://www.nhs.uk/Conditions/repairtotendon/Pages/Introduction.aspx
http://orthoinfo.aaos.org/topic.cfm?topic=a00297
http://orthoinfo.org/topic.cfm?topic=A00549
http://orthoinfo.aaos.org/icm/default.cfm?screen=icm004_s01_p1
Periprosthetic Fractures (Fractures around Hip & Knee Replacements)
Incidence of fractures around the hip and knee replacements is rare but seems to be on the rise due to more and more people having joint replacement surgeries. Depending on the nature of the fracture, this could be treated by internal fixation or by revision of the prosthetic replacement of the joint depending on the bone stock and whether there is loosening of the implant. Mr Rao specialises in these fractures and has technical expertise in managing them. He has done extensive studies in these fractures and research. He has been teaching on these fractures to peers. He has also published his work in peer reviewed journals and presented his work in different continents including Europe, America and Asia.
Useful links
http://orthoinfo.aaos.org/topic.cfm?topic=A00634

Periprosthetic fracture Hip

Revision Hip Replacement

Fixation of Periprosthetic fractures of hip

Fixation of Inter-prosthetic fracture

Periprosthetic fracture of Knee

Fixation of Periprosthetic fracture of Knee
Expertise in management of torn abductor muscles around hip after hip replacements.
Tears of the abductors muscles of hip can be an infrequent but debilitating complication after total hip arthroplasty. This can result in intractable pain on outer side of your hip, result in a limp with inability to walk without a crutch or stick and instability of the hip.
Mr. Rao has researched and devised a new technique to repair these muscles and has been successfully treated many patients with this technique.
Proximal Femoral replacement
Reconstruction of either complex periprosthetic fractures around loose hip and knee replacement prosthesis or loose hip and knee replacements itself with severe bone loss can be challenging. Proximal femoral replacement or distal femoral replacements are rarely needed for treating these complex scenarios especially when severe bone stock deficiency has encountered. These enable patients to get back on their feet quickly and return to function. Mr. Rao has expertise in carrying out these procedures and has been successfully doing these rare complex procedures.
Infected Hip replacement with bone loss and hip spacer in situ
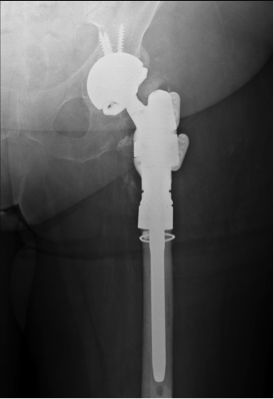
Proximal Femoral Replacement and acetabular reconstruction
Distal Femoral replacement for periprosthetic fracture
Mr Rao has done intensive work on management of fractures around knee replacements (periprosthetic fractures). His work included comparative study of Distal Femoral Arthroplasty/replacement’’ versus internal fixation for distal femoral periprosthetic fractures. Results showed better clinical outcomes in appropriate patients and helps them back on their feet quicker. This work has been presented in 34th SICOT Orthopaedic World Congress, British Association for Surgery of Knee, 2013 and due to be presented at ‘’American Association of Orthopaedic Surgeons Annual Conference’’ in San Diego, USA in March 2017.

Periprosthetic fracture of Knee

Distal Femoral Replacement
Management of simple and complex trauma of lower limb and upper limb fractures
Mr Rao is specialises in fractures of lower limb as well as of wrist, elbow and forearm. Private or insured patients with acute orthopaedic injuries requiring surgery are encouraged to use the private facilities available in Chichester suite at St Richard’s Hospital in Chichester.
|